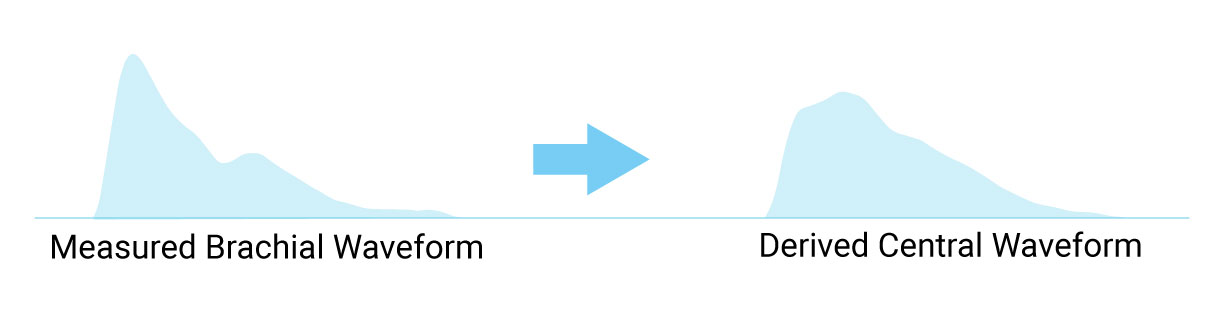
Central Blood Pressure is the pressure in the ascending aorta, just outside the left ventricle. It is the pressure that the target organs are exposed to and, due to arterial pressure amplification, is lower than brachial cuff pressures.
Blood pressure is not a constant force throughout the body. Numerous factors such as arterial stiffness affect the pressure wave as it travels from the aorta to the arm, making cuff pressure an unreliable indication of central pressure. As you age, your arteries stiffen and amplification is reduced.
Amplification of Blood Pressure Wave
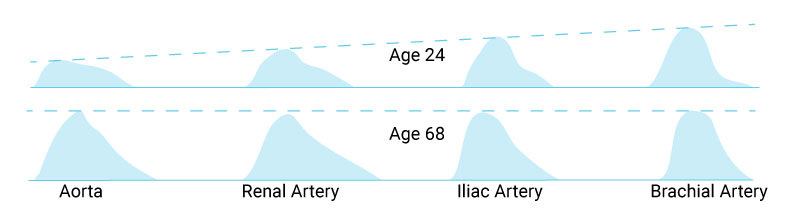
Central Blood Pressure Variation
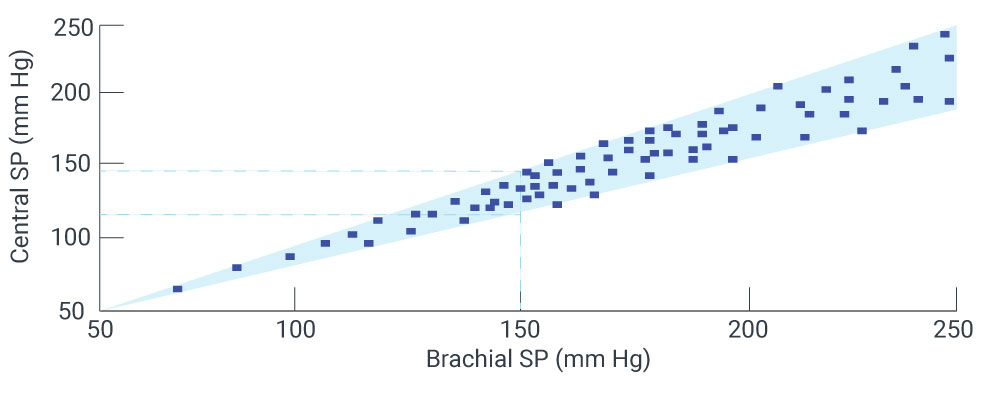
Systolic blood pressure is amplified by a level that varies greatly from patient to patient. Two individuals can have the same brachial cuff pressures but their central pressures can differ by >30mmHg.[1][2][3]
Augmentation Pressure: Central systolic and pulse pressures are increased in the presence of stiffer arteries, causing a higher ventricular after-load and energy used by the heart to pump to be wasted. Evaluation of the central pressure waveform contour allows for determination of augmentation pressure (AP) and the augmentation index (AIx), two parameters that quantify the increased pressure.
24-hour Central Blood Pressure: Oscar 2 with SphygmoCor combines the superior predictive power of Central Blood Pressure with the established standard for hypertension diagnosis providing a 24-hour study with up to 250 brachial and central blood pressure measurements.
Central Blood Pressure Applications
- Noninvasive central blood pressure assessments individualize treatment decisions and help get patients to goal.
- Hypertension management using central BP was associated with similar outcomes with less medication required.[4][5]
- Antihypertensive medications have differential effects on central vs. brachial blood pressure, which can explain variability in clinical outcomes.[6]
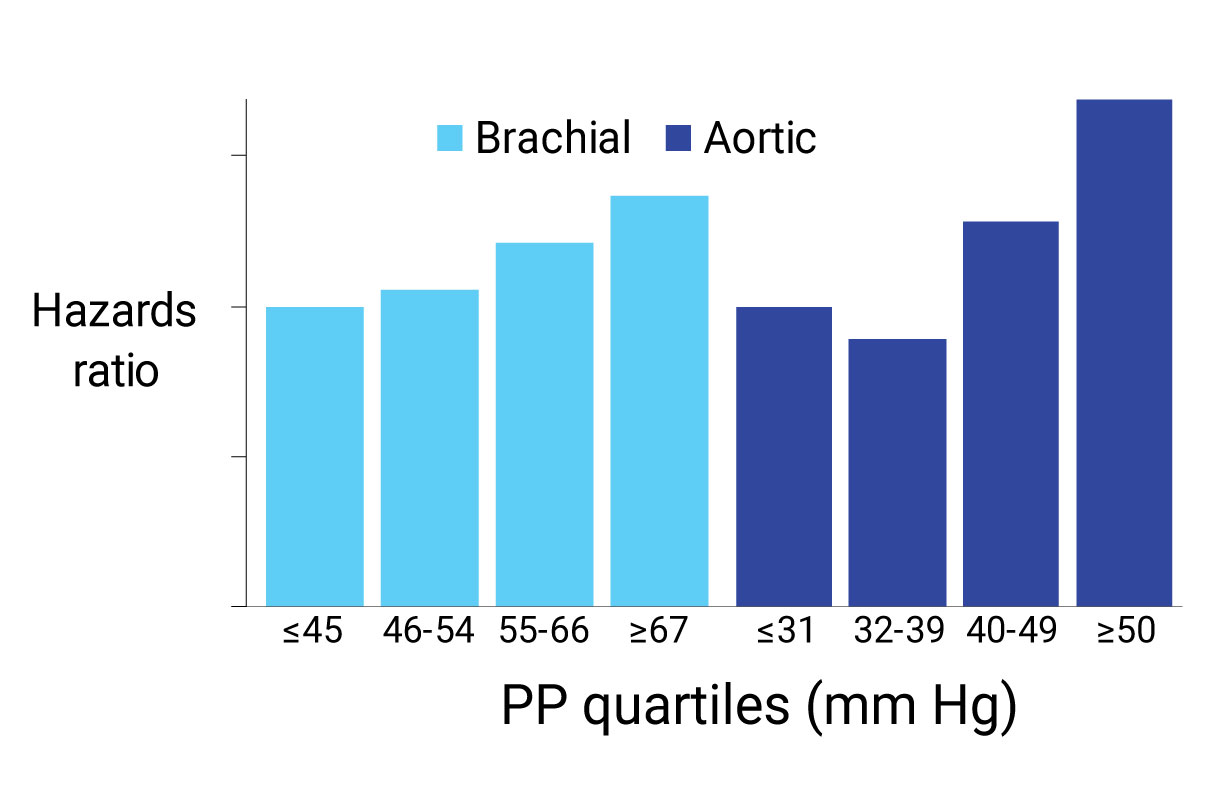
- Central blood pressure is more predictive of cardiovascular (CV) outcomes than brachial blood pressure, primarily due to proximity to target organs.[7]
Hypertension
A better predictor of outcome: A multi-year, NIH study in more than 3,500 high risk subjects demonstrated that central pulse pressure was more strongly predictive of CV events. Specifically, central pulse pressures > 50mmHG had a 20% increased risk of having a CV event in the next 5 years. Brachial pulse pressure did not show a similar threshold.[7]
Achieving similar outcomes with less medication: Research has also shown that using central blood pressure in addition to traditional 24-hour ABPM allows effective hypertension management with reduced necessary medication, particularly in younger patients.[4][5]
Chronic Kidney Disease
Augmentation Index as a predictor of mortality: Augmentation Index (AIx) has been shown to be a valuable tool in the management of end-stage renal failure patients. AIx was shown to be an independent predictor of cardiovascular and all cause mortality in a study of 108 end-stage renal failure patients.[8]
AIx has also been shown to be an independent predictor of all-cause and CV mortality in a meta-analysis of >5,000 subjects.[9]
Oscar 2 with SphygmoCor Inside


Why choose SphygmoCor?
It's the only device to provide a validated, fully-featured ascending aortic pressure waveform.
SunTech Medical has created the first and only ABP Monitor with SphygmoCor inside, providing the gold standard in non-invasive measurement of central blood pressure and arterial stiffness. The Oscar 2 ABPM system delivers a patient-focused solution with unmet comfort, data reliability and confidence.
How SphygmoCor Works
- Standard brachial blood pressure measurement is captured according to ABPM schedule

- Cuff inflates to sub-diastolic pressure for pulse waveform capture
- On-board SphygmoCor processor utilizes validated methodolgy to derive an ascending aortic pressure waveform
Transfer function has been validated in:
- Different disease states
- The presence of drug infusion
- During exercise
Utilized in more than 1,000 peer-reviewed publications with highly reproducible results.
References:
- O’Rourke et al. Br J Clin Pharmacol 2001;51:507-22
- Sharman JE et al J Hum Hypertens 2008 (12):838-44
- McEniery et al Hypertension 2008 6(51):1476-82
- Sharman et al. Hypertension. 2013 62:1138-45
- Kosmala et al. Am J Hypertens. 2015 108
- Williams B et al., Circulation 2006 113: 1213-25
- Roman, et al., JACC 2009 54:1730-4
- London GM Hypertension 2001 38:434-8
- Vlachopoulos et al. EHJ 2010 31(15):1819-1822